Modafinil and Heart Health: What You Need to Know
Modafinil, sold under the brand name Provigil, is a prescription medication approved for narcolepsy, shift work sleep disorder, and obstructive sleep apnea. It is known for promoting wakefulness without the extreme highs and crashes associated with traditional stimulants. As off-label use for fatigue and cognitive enhancement has grown, questions have emerged about how modafinil may affect heart health, particularly in people with cardiovascular conditions.
What Is Modafinil?
Modafinil is classified as a wakefulness-promoting agent. While its primary approvals are for sleep-related disorders, it’s increasingly being used off-label for conditions like multiple sclerosis-related fatigue and even as a cognitive enhancer. It differs pharmacologically from traditional stimulants, having a milder effect on dopamine pathways and a lower abuse profile (StatPearls, 2025).
How Modafinil Affects the Brain and Body
Modafinil’s mechanism of action includes:
- Inhibition of the dopamine transporter (DAT), increasing extracellular dopamine concentrations (De La Garza et al., 2011).
- Indirect activation of orexin, histamine, and norepinephrine systems, enhancing wakefulness without producing euphoric effects (StatPearls, 2025).
- Lack of significant interaction with serotonin or direct adrenergic agonism, making it pharmacologically distinct from amphetamines (StatPearls, 2025).
Modafinil’s Impact on Blood Pressure and Heart Rate
Several clinical studies and observational trials indicate that modafinil can cause mild increases in heart rate and blood pressure, particularly in individuals already predisposed to cardiovascular disease. For most healthy adults, these changes are not clinically significant (FDA, 2015).
Risks of Heart-Related Side Effects
Though uncommon, more serious cardiovascular effects have been reported:
- Palpitations and arrhythmias
- Chest pain and hypertension
- Rare cases of myocardial infarction or stroke in high-risk individuals
In a large-scale analysis across three U.S. health databases, researchers found no overall increased risk for myocardial infarction or cardiovascular hospitalization. However, OSA patients with a history of stroke showed nearly double the risk of recurrent stroke when using modafinil (Kaplan et al., 2018).
Modafinil in Patients with Pre-existing Heart Conditions
Modafinil should be used cautiously in individuals with:
- Uncontrolled hypertension
- Arrhythmias
- Prior stroke or heart attack
The FDA advises that cardiovascular screening be performed before initiating modafinil in patients with risk factors. Regular monitoring of heart rate, blood pressure, and ECG may be warranted during treatment (FDA, 2015).
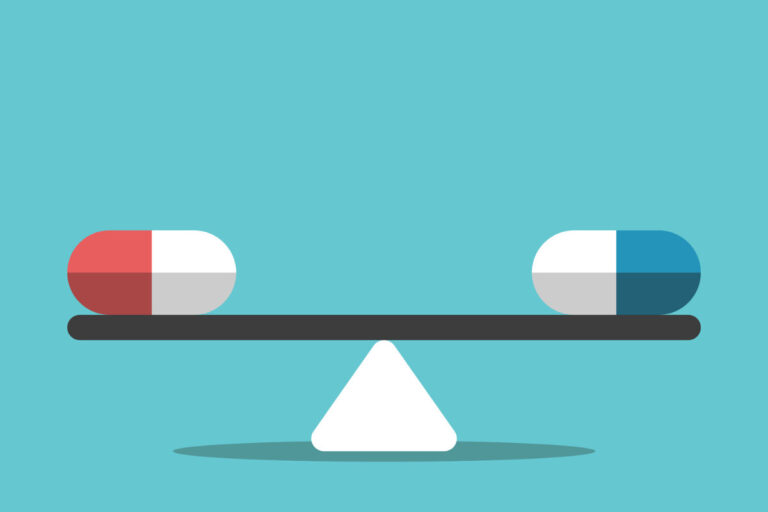
Comparing Modafinil to Other Stimulants
| Feature | Modafinil | Amphetamines | Caffeine |
|---|---|---|---|
| Blood Pressure Impact | Mild | Moderate to High | Mild to Moderate |
| Addiction Potential | Low | High | Low to Moderate |
| Onset of Action | Gradual | Rapid | Rapid |
| Euphoria | Rare | Common | None |
Modafinil is often favored for long-term use due to its lower abuse liability and more stable cardiovascular profile (De La Garza et al., 2011).
Recommendations for Monitoring and Use
Healthcare providers should:
- Conduct baseline cardiovascular evaluation before prescribing modafinil
- Monitor BP and heart rate periodically, especially during dose adjustments
- Educate patients about symptoms like chest pain, dizziness, or irregular heartbeat
Patients with stroke history or cardiac arrhythmias should only use modafinil under specialist supervision.
Patient Perspectives and Anecdotal Reports
Some users report improved productivity and cognitive clarity, while others mention episodes of rapid heartbeat or mild chest discomfort. While anecdotal reports can offer context, they are not substitutes for peer-reviewed clinical data. Always consult a medical professional before initiating or discontinuing use.
Conclusion
Modafinil is highly effective for managing excessive sleepiness and fatigue, yet it requires careful use in individuals with cardiovascular concerns. Research indicates that it is typically safe for the heart in healthy users, but caution is recommended for anyone with a previous heart attack, arrhythmia, or stroke. When patients are screened and monitored appropriately, modafinil can be used safely and effectively.
References
- U.S. Food and Drug Administration. (2015). PROVIGIL® (modafinil) tablets, for oral use, C-IV [Prescribing information]. U.S. Department of Health and Human Services. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020717s037s038lbl.pdf
- Greenblatt, K., & Adams, N. (2023). Modafinil. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK531476/
- De La Garza, R., Zorick, T., London, E. D., & Newton, T. F. (2010). Evaluation of modafinil effects on cardiovascular, subjective, and reinforcing effects of methamphetamine in methamphetamine-dependent volunteers. Drug and Alcohol Dependence, 106(2–3), 173–180. https://doi.org/10.1016/j.drugalcdep.2009.08.013
- Kaplan, S., Goehring, E. L., Jr., Melamed-Gal, S., Nguyen-Khoa, B. A., Knebel, H., & Jones, J. K. (2018). Modafinil and the risk of cardiovascular events: Findings from three US claims databases. Pharmacoepidemiology and Drug Safety, 27(11), 1182–1190. https://doi.org/10.1002/pds.4642